Continued from previous article
The key purpose of the Telecom Bill is regulating the Telecom industry . Accordingly Chapter 3 covers Licensing, Registration, Authorization and Assignment.
The first point to be noted is the “Exclusive Privilege” created for the Government to provide tele communication services within India including setting up of the telecommunication network and use and assignment of spectrum. The license will be subject to terms and conditions which becomes the basis of operation and determination of other obligations under the Act.
It is necessary to note that even possession of a wireless equipment requires authorization. Wireless equipment under the Act means
“any telecommunication equipment used or capable of use in wireless communication, including any wireless transmitter that is capable of use for broadcasting or emission of wireless communication”
Since the definition is broad and may cover even a wireless router and mobile, the Government needs to provide an exemption list while notifying the Act.
Similarly the possession of any equipment that can block tele communication is prohibited.
Possession of equipment that can pick “off the air telecommunication signals” also needs to be subject to strict licensing. Such equipment is used for surveillance by intelligence agencies and by unauthorized agencies.
An interesting provision is that
“Any entity which is granted a license under sub-clause (2) of Section 3, shall unequivocally identify the person to whom it provides services, through a verifiable mode of identification as may be prescribed.”
“The identity of a person sending a message using telecommunication services
shall be available to the user receiving such message, in such form as may be prescribed, unless specified otherwise by the Central Government.”
The above provisions should be read with the wide definition of telecommunication services which states
“telecommunication services” means service of any description (including broadcasting services, electronic mail, voice mail, voice, video and data communication services, audiotex services, videotex services, fixed and mobile services, internet and broadband services, satellite based communication services, internet based communication services, in-flight and maritime connectivity services, interpersonal communications services, machine to machine communication services, over-the-top (OTT) communication services) which is made available to users by telecommunication, and includes any other service that the Central Government may notify to be telecommunication services;
This means that in both E-Mail and Mobile services, the identity of the sender of the message should be available to the receiver.
This will put an end to the menace of fake E-Mails and Fake Voice calls at least to a substantial extent.
We will wait and see how the Gmail or WhatsApp will respond. Presently they are using “Anonymization” as a right and using “Privacy” as a fig leaf to let criminals act through their platforms. This should stop and probably they will oppose this provision as they did when it was first proposed in PDPB 2019. Even the domain name registrars have the tendency to hide the identity of the registrants on the pretext of Privacy and facilitate frauds of phishing etc.
We welcome this provision whole heartedly. At the same time, in order to make “Privacy” available through “Pseudonymization”, we have proposed “Regulated Anonymity” proposed by Naavi way back in 2012. May be this should be considered with some modification now and TRAI should provide it as an option under the rules.
…to be continued
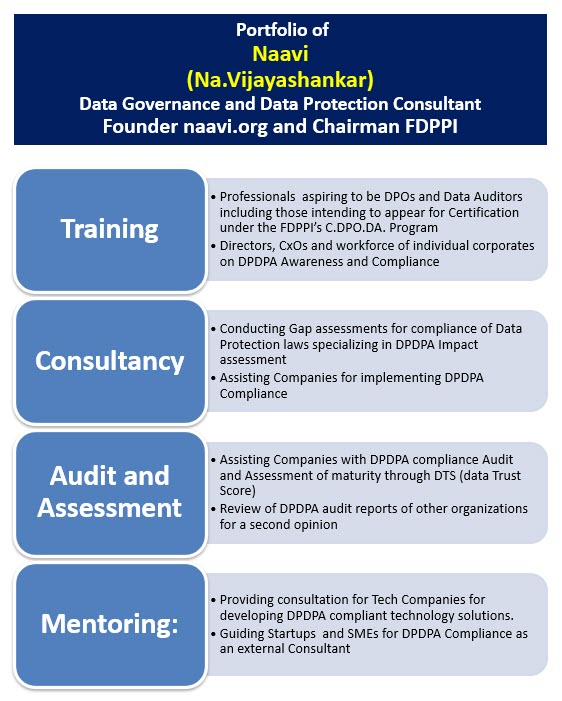
Naavi